|
| by Sally Fansler, PT |
As discussed in one of our previous blogs, Illinois is now a direct access state, which allows patients to attend physical therapy without a referral from a doctor. This access allows for greater autonomy for both patients and therapists in our state. Since this legislation is only a little over a year old, however, word travels slowly, and many of our patients are not aware of the choices they have when seeking medical care.
Prior to this advancement in 2018, restrictions on direct access proved to delay the healing process for patients and increase medical expenses by requiring a separate consultation and often additional testing. Patients would often be delayed weeks in beginning their treatment due to the need to schedule an appointment with their primary care physician, and patients who did not have a primary care physician would have to navigate the process of finding someone and becoming a new patient. By making physical therapy more accessible to patients, direct access allows physical therapists to treat patients immediately, leading to more expedient improvement.
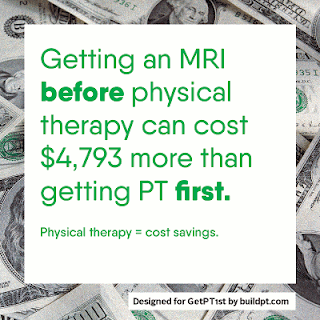
Furthermore, multiple research studies have agreed on the benefits of direct access. A study from Georgetown and Johns Hopkins University found that the total paid averaged $2236 for “physician referral” episodes of physical therapy as compared to $1004 for “direct access” episodes of physical therapy. Additionally, the physician referral episodes were 65% longer in duration than the direct access episodes. A similar study from the Journal of Health Services Research analyzed patients with low back pain. Those who saw a physical therapist at the first point of care had an 89% lower probability of having an opioid prescription and a 28% lower probability of having any advanced imaging services. The pattern is clear - lower cost, quicker improvement, and positive outcomes.
Direct access for physical therapy in Illinois has been a long time in the making, and has only been made possible through the expense, time, energy and effort on the part of physical therapists and physical therapy advocates throughout the U.S.to finally allow consumers (like you!) prompt access to physical therapy services. We are confident that, with fewer barriers, our patients will choose P.T. first!
Call to Action:
Spread the word!
At Lakeshore Physical Therapy, we are honored when our patients exercise their right to direct access care from our experienced physical therapists that are fully invested in their progress.
Resources:
Denniger T. et al. (2017). The Influence of Patient Choice of First Provider on Costs and Outcomes: Analysis From a Physical Therapy Patient Registry. Journal of Orthopaedic & Sports Physical Therapy, 2017, Volume:48 Issue:2 Pages:63-71 doi: 10.2519/jospt.2018.7423
Mitchell J. (1997). A Comparison of Resource Use and Cost in Direct Access Versus Physician Referral Episodes of Physical Therapy. Physical Therapy, Volume 77, Issue 1, 1 January 1997, Pages 10–18, doi.org/10.1093/pti/77.1.10
Frogner B. (2018). Physical Therapy as the First Point of Care to Treat Low Back Pain: An Instrumental Variables Approach to Estimate Impact on Opioid Prescription, Health Care Utilization, and Costs. Health Services Research, 2018 Dec;53(6):4629-4646. doi: 10.1111/1475-6773.12984. Epub 2018 May 23.